Sickle Cell Disease (SCD)
How important are safe, compatible blood transfusions for people living with sickle cell?
Transfusions for patients with sickle cell disease (SCD) are vital for their health and well-being.
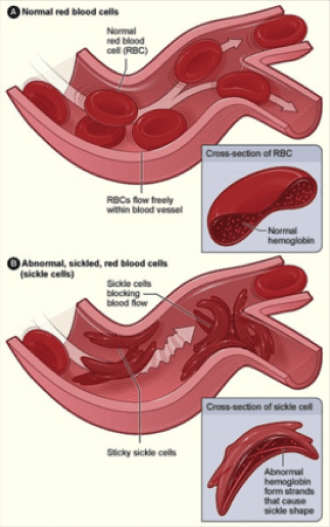
SCD is an inherited blood disorder affecting the red blood cells. It causes red blood cells to become rigid and crescent (or sickle) shaped, making it difficult for blood to properly circulate.
Disease complications can severely impact a patient’s way of life and interfere with day-to-day activities. Complications can include strokes, anemia, debilitating pain episodes, chronic fatigue, swelling in the hands and feet, severe infections, jaundice, organ damage and failure, and even death.
There is no cure for sickle cell disease, though transfusions help manage symptoms and improve quality of life. Patients with SCD can require frequent blood transfusions for their entire lives, beginning in early childhood. Each transfusion could require from one to 10 units of red blood cells, depending on the patient’s age and size.
Most sickle cell patients in the United States are Black/African American. The disease also occurs in people of Latin American, Mediterranean, South Asian and Middle Eastern heritage.

Compatible blood for sickle cell patient support is more likely found among blood donors who share the patient’s race or ethnicity. It is essential that Black/African American donors are well represented among Carter BloodCare’s volunteer donors; this gives patients and their physicians greater confidence in compatible blood being available.
Testing blood beyond groups A, B and O
Medical Director Dr. William Crews explains there are more blood groups than just A, B and O types. Among additional subgroups is where blood centers find the most compatible match for sickle cell patients and others requiring a complex match.
Importance of R0 to people with sickle cell disease
R0 donors are in demand to help patients living with sickle cell disease. Learn about the R0 subtype.